 Continuing to perform well means engaging in lifelong learning. For surgeons, this is crucial for the timely recognition and reduction of patient safety risks. Research on learning in practice often adopts the lens of self-regulated learning (SRL), which consists of a cyclical model of preparation (setting goals, planning, choosing an approach), execution, and reflection. Self-regulated learning has been shown to be more effective for individuals with a growth mindset: those who believe that abilities and intelligence can be developed through effort. In contrast are those who are convinced that abilities and capacities are innate and therefore unchangeable: the fixed-mindset individuals. To add a necessary nuance: mindset is, of course, not a dichotomous phenomenon, and it also appears to be context-dependent. Still, research has shown that a growth mindset enhances both learning capacity and motivation. As everyone knows from experience, motivation is key when it comes to learning, with intrinsic motivation resulting in the best possible performance.
Continuing to perform well means engaging in lifelong learning. For surgeons, this is crucial for the timely recognition and reduction of patient safety risks. Research on learning in practice often adopts the lens of self-regulated learning (SRL), which consists of a cyclical model of preparation (setting goals, planning, choosing an approach), execution, and reflection. Self-regulated learning has been shown to be more effective for individuals with a growth mindset: those who believe that abilities and intelligence can be developed through effort. In contrast are those who are convinced that abilities and capacities are innate and therefore unchangeable: the fixed-mindset individuals. To add a necessary nuance: mindset is, of course, not a dichotomous phenomenon, and it also appears to be context-dependent. Still, research has shown that a growth mindset enhances both learning capacity and motivation. As everyone knows from experience, motivation is key when it comes to learning, with intrinsic motivation resulting in the best possible performance.
Okay, so SRL, mindset, and motivation are interrelated. In this study by Kirsten Dabekaussen et al., we set out to disentangle these relationships. More specifically, our question was what role motivation plays in the relationship between mindset and SRL. What we found is that surgeons with a strong growth mindset more frequently went through all three phases of SRL. We also found that SRL was not directly affected by a fixed mindset, but rather indirectly through lower levels of intrinsic motivation. The figure summarizes the results. These can, of course, be explored in detail in the publication in Perspectives on Medical Education.
What an incredibly instructive and enjoyable week it was with colleague Prof. Karen Mattick (University of Exeter, UK), who spent the entire week at Amsterdam UMC as a Spinoza Visiting Professor, generously sharing her knowledge and experience. Karen Mattick is Professor of Medical Education and an expert in the wellbeing of healthcare professionals. I have been running into her for years at (international) conferences and have always been impressed by her sharpness, vision, expertise, and (British) sense of humour. When she responded positively to the invitation to come to Amsterdam, we—together with a number of Amsterdam UMC colleagues—put together a varied programme with insightful sessions for, among others, PhD students, medical education researchers, educational leaders, those interested in women’s wellbeing (in particular menopause), and the wider public.
 In the photo, Karen is teaching researchers about the realist approach: an approach that teaches us to always study problems and interventions in their context. In other words, we should not limit ourselves to the question “what works,” but more often ask “what works for whom, under which circumstances.” Food for thought—and a call for meaningful research!
In the photo, Karen is teaching researchers about the realist approach: an approach that teaches us to always study problems and interventions in their context. In other words, we should not limit ourselves to the question “what works,” but more often ask “what works for whom, under which circumstances.” Food for thought—and a call for meaningful research!
Another thing I learned from Karen Mattick is the power of cartoons in communication (though it’s worth remembering that not every audience will appreciate them). Many also heard her important warning that wellbeing interventions can actually cause harm (!) if they are not aligned with the needs and wishes of healthcare professionals. More is certainly not automatically better. Offering coaching, mindfulness, and/or team outings is no solution to an inefficient organisation or overly complex administrative and IT systems.
We are far from done talking or thinking this through. The collaboration with Karen M will continue. I am already looking forward to it!
Almost 20 years ago, the Netherlands began thinking about the individual performance assessment of medical specialists (IFMS). After years of focusing on quality assurance by and within professional groups —culminating in a solid system of visitatie (peer reviews)—it became clear that the individual medical specialist could no longer be left out of the equation. In line with international developments, a system of IFMS was also introduced in the Netherlands. Thoughtfully developed, well-considered, and based on scientific evidence and consensus. The latter was achieved through a two-year project involving multiple medical societies and pilot studies in both large and small hospitals. The recommendations for introducing IFMS, written by the so-called IFMS Committee (commissioned by the Dutch Order of Medical Specialists), was published in the report “Persoonlijk Beter”. As project advisor, I co-authored most of this report together with the then-chairman, Professor Dr. Berry Kremer.
Although ‘development’ often—and in this case too—progresses faster than ‘implementation’, IFMS gradually found its way into practice in the years following the report’s publication in 2007. Fast forward to 2025: all medical specialists are now familiar with the system of (guided) reflection on their own performance, including the 360-degree feedback that is collected for this purpose, and the subsequent reflection dialogue. This “100% participation” is not surprising, as since 2020, participation has been mandatory for individual (once every five year) recertification purposes.
We can now state that IFMS is here to stay. As one of the IFMS facilitators—those who conduct the reflection conversations with medical specialists—I am pleased about this. Humbly, I believe I have had many meaningful conversations with medical specialists. Meaningful in the sense of creating a positive experience by taking two full hours to truly listen (nonjudgmentally—that’s what I try at least), to exchange ideas, and to think constructively and appreciatively about a personal development goal. Meaningful also in terms of a tangible result: when we together formulate a goal and action points that are important and achievable for the physician, and for which they are genuinely motivated.
I consider it an honor when specialists choose to have these conversations with me. I am consistently impressed by the immense talent working at Amsterdam UMC and the strong commitment to providing excellent care for patients, and to supporting colleagues. At the same time, I also observe much distress: organizational struggles—with leadership, social safety, the consequences of the merger—as well as personal struggles with insecurity, ambitions, and life questions.
There is a lot to be said about IFMS. And it is good that we start saying it, based on research. What forms have developed? What do specialists think about it? How do they experience receiving feedback from colleagues? What touches them, what paralyzes them, what motivates them to act—or to refrain from action? Are all facilitators as positive as I am? And, of course, the key question: what does it all lead to?
My new PhD candidate, Eva Theodoropoulou, will be exploring these questions in the coming years. After 20 years, it is time.
 With all the attention and innovations in residency training , program directors (PD) and supervisors have taken on a significant number of additional tasks and responsibilities. This could not—and cannot—happen without considerable focus on faculty development: activities that teaching faculty undertake to improve their knowledge, skills, and behaviors as educators, teachers and supervisors. These activities have been strongly supported by the emergence of learning centers (Leerhuizen), the expanding range of professional development offerings, and numerous thematic conferences—including the assessment and evaluation of the knowledge and skills gained (think of site visits, training climate surveys, feedback from residents, etc.).
With all the attention and innovations in residency training , program directors (PD) and supervisors have taken on a significant number of additional tasks and responsibilities. This could not—and cannot—happen without considerable focus on faculty development: activities that teaching faculty undertake to improve their knowledge, skills, and behaviors as educators, teachers and supervisors. These activities have been strongly supported by the emergence of learning centers (Leerhuizen), the expanding range of professional development offerings, and numerous thematic conferences—including the assessment and evaluation of the knowledge and skills gained (think of site visits, training climate surveys, feedback from residents, etc.).
Nevertheless, increasingly more is being asked and expected of teaching faculty. As is typical for doctors, they do their best to meet these expectations—as well as they can. The result is impressive: as of 2025, terms such as competency-based education, portfolios, EPAs (Entrustable Professional Activities), mini-CEXs (Korte Klinische Beoordelingen), individualization, and training plans have become familiar vocabulary for medical specialists with a teaching role.
But there are limits.
 While the professionalization of didactic expertise is, of course, never “finished,” additional demands are being placed on teaching faculty on top of their current commitments. After all, high-quality training is influenced by workforce shortages, the threatened (and experienced) work-life balance, insufficient alignment between education and clinical care, part-time work and scaling up, increasing bureaucratization, healthcare digitalization, and financial constraints. Faculty cannot (unfortunately) keep all of these developments out of residents’ learning environment. And so, they must deal with them.
While the professionalization of didactic expertise is, of course, never “finished,” additional demands are being placed on teaching faculty on top of their current commitments. After all, high-quality training is influenced by workforce shortages, the threatened (and experienced) work-life balance, insufficient alignment between education and clinical care, part-time work and scaling up, increasing bureaucratization, healthcare digitalization, and financial constraints. Faculty cannot (unfortunately) keep all of these developments out of residents’ learning environment. And so, they must deal with them.
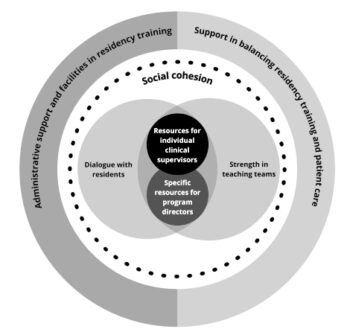
But “they” does not refer solely to the individual trainer—or perhaps even to the trainers’ group. PD’s and supervisors can only function optimally if they are optimally supported in their educational role and tasks. That is why it is time to shine a spotlight on the teaching climate, a concept we coined in the accompanying article in Academic Medicine. In Defining a Supportive Teaching Climate for Clinical Supervisors in Residency Training, researchers Anne van Graafeiland et al. present what (head) trainers consider to be a constructive teaching climate.
 There is much concern about the well-being of doctors. Fortunately, there is also much attention to this well-being. This started long before the COVID-19 pandemic, intensified during the pandemic, and has now become a high, if not the highest, policy priority for hospital administrators and other healthcare institutions. However, high priority does not necessarily equate to effectiveness. In the ‘first phase’, healthcare professionals were overwhelmed with a variety of individual interventions for well-being, such as coaching, mindfulness courses, meditation training, etc. I am a fan of all of them and believe it is a benefit that they are available to professionals if desired; anyone can benefit from them. In my own life, I’ve consumed a fair amount of ‘personal development,’ even long before it became a trend, let alone being offered by healthcare institutions. I believe I have learned important (life) skills from it, and that I have become more self-aware, a bit wiser, more resilient, and maybe even more fun person. The investments I made—time, growing pains, and money—were and still are my own choice. The more mature version of myself is what I bring into the world, and (therefore also) into my work. Just as others do who choose to walk the path of development.
There is much concern about the well-being of doctors. Fortunately, there is also much attention to this well-being. This started long before the COVID-19 pandemic, intensified during the pandemic, and has now become a high, if not the highest, policy priority for hospital administrators and other healthcare institutions. However, high priority does not necessarily equate to effectiveness. In the ‘first phase’, healthcare professionals were overwhelmed with a variety of individual interventions for well-being, such as coaching, mindfulness courses, meditation training, etc. I am a fan of all of them and believe it is a benefit that they are available to professionals if desired; anyone can benefit from them. In my own life, I’ve consumed a fair amount of ‘personal development,’ even long before it became a trend, let alone being offered by healthcare institutions. I believe I have learned important (life) skills from it, and that I have become more self-aware, a bit wiser, more resilient, and maybe even more fun person. The investments I made—time, growing pains, and money—were and still are my own choice. The more mature version of myself is what I bring into the world, and (therefore also) into my work. Just as others do who choose to walk the path of development.
But personal growth is not the answer to the increasing work stress caused by the ever-more complex and demanding conditions that healthcare professionals have to work in. Organizations must also take action. Healthcare institutions must invest—time, growing pains, and money—in becoming more self-aware, wiser, more resilient, and, if possible, more enjoyable. It is time for the ‘second phase’ of caring for healthcare professionals. Well-being researchers and healthcare professionals have been calling for this for years. Administrators also recognize the necessity, if only because the ad hoc approach has proven to be exhausted. On a macro level, this requires a courageous conversation where all stakeholders in healthcare must come to the table: umbrella organizations, health insurers, professional associations, and—last but not least—the government. Courageous because there is much truth in the cry for help, ‘the system needs to change.’
Meanwhile, the (hospital) business must go on, and the conversation about well-being is more relevant than ever. A conversation indeed at the level where influence can be exerted. For doctors, that circle of influence is the medical department. What can relieve pressure for the individual doctor? What can provide simple relief in the immediate environment? Does everything have to be done immediately? How can colleagues support each other? Are there colleagues who are ‘on the edge,’ struggling with their private lives, or feeling unsafe within the team? Is everyone in the group seen? Is there enough laughter? Do team members appreciate each other and, if so, how do they show it?
Sharing is caring. If teams want to have a meaningful conversation about the well-being experienced within their department but do not want to start completely from scratch, one option is to begin the discussion using the results of a brief screening, conducted with the help of the WellNext Scan (WNS). This Scan has been developed and tested over the past few years by my department, PP&CC. The WNS is based on the latest literature, surveys of doctors’ needs, and practical use by groups of medical specialists and residents. The scientific results can be read in this publication by Sofiya Abedali et al. in PLoS One.
The Trump administration is leaving a trail of destruction through American science with its war on ‘woke’. The consequences are also being felt in the Netherlands. In a letter to the editor published today in the Volkskrant, signed by 300 scientists, healthcare professionals, and other experts, universities, policymakers, and the government are urged to continue supporting researchers and to safeguard high-quality and inclusive healthcare for everyone. I wholeheartedly added my signature to this letter. You can still show your support by signing the petition.
 Today’s Netherlands Medical Journal reports that the path to professorship is still more often successful for male doctors than for their female colleagues. Colleagues from ErasmusMC published this well-underpinned supported research finding regarding gender differences in medical science. The largest explanatory factor (55%) they found was the number of publications. There was no difference between men and women in terms of the number of successful grant applications.
Today’s Netherlands Medical Journal reports that the path to professorship is still more often successful for male doctors than for their female colleagues. Colleagues from ErasmusMC published this well-underpinned supported research finding regarding gender differences in medical science. The largest explanatory factor (55%) they found was the number of publications. There was no difference between men and women in terms of the number of successful grant applications.
As board member of the Dutch Women Professors, I was asked to reflect on these findings for the Dutch national newspaper Volkskrant in an interview with journalist Erna van Dalen. Lidwien Poorthuis, director of the Dutch Women Professor, was interviewed about the same study for Radio 1, News Weekend. The findings are not new for the Network; in the annual Monitor Female Professors – the report on the representation and progression of female scientists – we have been reading for years about persistent inequality between male and female scientists. Medical faculties currently have just over 30% female professors. This percentage is increasing, but too slowly. While lecture halls and the scientific pipeline are more than filled with women, it is still the men who more frequently move on to higher leadership, decision-making, and culture-defining positions. To achieve the desired equality between men and women more quickly, it is essential to change the appointment system and the dominant masculine culture within the university medical centers (UMCs). The fact is that female department heads are underrepresented in all UMCs (ranging from 14.7% to 42%); the current culture bearers at the department level are mostly men. Professors are typically nominated by the department leadership. Programs such as ‘Acknowledgment & Recognition’ aim to make this culture – and thus the system – more diverse by, for example, broadening appointment criteria. Not only the grant application success rates and the H-index (publication numbers) of scientists should weigh in the decision, but also other important aspects for the academy, such as teaching efforts, academic duties, societal impact, and good leadership of research teams.
We wondered if, when, and how residents feel valued in the workplace. In other words, how do residents appreciate appreciation? This interview study by Rosa Bogerd et al. provided some important answers, valuable insights, and a nuanced view of appreciation. Peers, patients, and supervisors can make residents feel valued. This can be through a word, a question, a positive outcome, a thank you, a compliment, or even by giving them additional responsibilities. Whether, and to what extent, something is experienced as feeling valued depends on the timing of the expressed appreciation and the values that are important to the resident.
For colleagues, supervisors, and trainers who want to express more appreciation, and bring positivity to the workplace, the reported experiences of residents may be useful. See this Academic Medicine publication Appreciating Appreciation: Residents Experience Feeling Valued Differently as Learners, Physicians and Employees.
In delivering the Anatomical Lecture, British professor Sadaf Farooqi, Professor of Metabolism and Medicine at the University of Cambridge, educated around 2,000 people on the genetic causes of obesity. The pre-program was designed as both “learning and amusement.” It’s no longer news that the industry entices us to consume unhealthy, (literally) disease-causing products, but it is still surprising that stronger actions are not being taken. Fortunately, Trijntje Oosterhuis serenaded us with her rendition of What the world needs now…. in the always impressive Royal Concertbuilding.
 What is WellMed? A conference about the well-being of healthcare professionals that also energizes you. Through the passionate and knowledgeable colleagues, the hospitality of the Greeks, and the beautiful surroundings (see photo: the Velos area, located between Athens and Thessaloniki). “Conference” might not be the right word; it was more of a meeting with about 50 participants who spent three days discussing the causes of reduced well-being among healthcare professionals and effective solutions. After 10 years of WellMed, much has been achieved and much is worth sharing. It is clear that well-being as a theme for research and policy no longer needs to be advocated for—it is receiving the recognition and attention it deserves. However, the decline in well-being (psychological ill health) among doctors and other healthcare professionals is not solved yet. New evidence on “what approach works in which context” (a strong argument for realistic approaches from our English colleagues) is hopefully bringing us closer to solutions. I’m happy to contribute with research and collaboration.
What is WellMed? A conference about the well-being of healthcare professionals that also energizes you. Through the passionate and knowledgeable colleagues, the hospitality of the Greeks, and the beautiful surroundings (see photo: the Velos area, located between Athens and Thessaloniki). “Conference” might not be the right word; it was more of a meeting with about 50 participants who spent three days discussing the causes of reduced well-being among healthcare professionals and effective solutions. After 10 years of WellMed, much has been achieved and much is worth sharing. It is clear that well-being as a theme for research and policy no longer needs to be advocated for—it is receiving the recognition and attention it deserves. However, the decline in well-being (psychological ill health) among doctors and other healthcare professionals is not solved yet. New evidence on “what approach works in which context” (a strong argument for realistic approaches from our English colleagues) is hopefully bringing us closer to solutions. I’m happy to contribute with research and collaboration.

A wonderful end to the summer holidays and a great start to the new (academic) year: the Rogano meeting. Our annual scientific conference on research in medical education. A summery snapshot with colleagues Ellen Ricke, Anne van Graafeiland, and Sofiya Abedali. The scientific results will follow later.
Once again, a study reports a quality difference in patient outcomes between female and male specialists. This study was published today in Annals of Internal Medicine. The evidence of the impact of a treating physician’s gender on patient clinical outcomes is growing stronger. This study also shows that female patients, in particular, benefit from being treated by a female specialist. The question of why these consistently reported differences exist is becoming increasingly pressing. The popular science magazine Quest.nl covered this publication, and I was asked to comment on the study (in Dutch).
Great, finally a male perspective on the discussion about the performance of male and female doctors. None other than dr Bert Keizer, physician and philosopher, opens his column in the Dutch newspaper Trouw with an intriguing scenario, presented in the title: The nightmare of a man with prostate problems is a female doctor. With his sharp and humorous voice, he discusses the interview with me published earlier (see December 18th) in the NTvG. I am happy with his support and critical reflections.

As with many, my new year started with a phone full of messages. On January 1st, I received many good wishes for 2024 from family and friends. But today, January 2nd, it was mainly reactions to a big interview in the AD about women and female qualities in healthcare.
Large clinical studies show that female patients are ‘better off’ if they are helped by a female medical specialist; this has been demonstrated for surgeons (based on research into 25 different surgical procedures), cardiologists (study of patients who present with a heart attack at the emergency department) and internists (research into 8 most common internal diagnoses). ‘Better off’ means hard patient outcomes such as fewer complications, fewer readmissions and lower mortality rates. The studies I refer to are done with American, Canadian and Swedish data. Sometimes the differences between male and female doctors are large and (also clinically) relevant, other times small, but always significant and consistent in favor of women.
Yet the question is not a men-versus-women issue. We do need to (want to) investigate what can be learned from the observed differences. For men and women. And also the unequal appreciation of male versus female qualities is more than worth discussing. Why? Because all human qualities are important for being able to provide good patient care. I spoke about these topics with AD journalist Ellen van Gaalen. It became a page-wide story (in Dutch). On January 3rd, the interview appeared in Het Parool.
NPO1 radio picked up the article and talked about it further in the Fact & Fiction section (EenVandaag). Listen here.
 At the end of the year, the Dutch Medical Journal – NTvG – discusses ‘tipping points’ in care and society. In an interview (in Dutch) with Rosie Sikkel, I spoke about the shift to more women and ‘female qualities’ in medicine. The latter is especially necessary. ‘Female qualities’ – such as listening, empathizing, compassion and intuition – were long attributed to women, but men and women can of course be compassionate, comforting and really empathize with the patient in front of them. It is important that we also appreciate these human qualities as indispensable for good and effective care, and (therefore) pay more attention to them in the training. Not as an ‘extra’ or ‘nice to have’ or ‘optional’, but simply because there is scientific evidence that these qualities are good for patient outcomes and good for the care professionals.
At the end of the year, the Dutch Medical Journal – NTvG – discusses ‘tipping points’ in care and society. In an interview (in Dutch) with Rosie Sikkel, I spoke about the shift to more women and ‘female qualities’ in medicine. The latter is especially necessary. ‘Female qualities’ – such as listening, empathizing, compassion and intuition – were long attributed to women, but men and women can of course be compassionate, comforting and really empathize with the patient in front of them. It is important that we also appreciate these human qualities as indispensable for good and effective care, and (therefore) pay more attention to them in the training. Not as an ‘extra’ or ‘nice to have’ or ‘optional’, but simply because there is scientific evidence that these qualities are good for patient outcomes and good for the care professionals.
 As expected, Maarten Debets defended his impressive and relevant book, Physicians Enhancing Their Professional Performance, with great skill. Here is the radiant new young doctor, along with his equally radiant PhD thesis committee: Dr. Milou Silkens, Dr. Karen Kruijthof, and myself. Many thanks to all the opponents: Prof. Eva Knies (UU), Prof. Bart van Berden (UvT, not pictured), Prof. Hans Goudoever (UvA), Prof. Christiaan Vinkers (VU), Prof. Joris van der Post (UvA), and Prof. Suzanne Geerlings (UvA).
As expected, Maarten Debets defended his impressive and relevant book, Physicians Enhancing Their Professional Performance, with great skill. Here is the radiant new young doctor, along with his equally radiant PhD thesis committee: Dr. Milou Silkens, Dr. Karen Kruijthof, and myself. Many thanks to all the opponents: Prof. Eva Knies (UU), Prof. Bart van Berden (UvT, not pictured), Prof. Hans Goudoever (UvA), Prof. Christiaan Vinkers (VU), Prof. Joris van der Post (UvA), and Prof. Suzanne Geerlings (UvA).
This is what team work looks like. What a continuous challenge to align patient care and educational goals. In a previous publicatie in Academic Medicine we addressed the efficient use of clinical performance data, by using known data from the EHR for residents’ assessment and feedback. In this new publication, under the leadership of dr Alina Smirnova, PhD, we test cased our own ideas for two clinical paediatric illnesses. Spoiler alert: this study contains new perspectives to positively impact patient care and residency training.
 Today Iris Jansen convincingly defended her PhD thesis, titled: Interactions that Matter: Understanding Residents’ Professional Growth Through Workplace Relationships. Please go read this impressive work here. This picture shows the all female research team: dr Milou Silkens, PhD en dr Renee Stalmeijer, PhD as Iris co-supervisors, and myself as Iris proud supervisor.
Today Iris Jansen convincingly defended her PhD thesis, titled: Interactions that Matter: Understanding Residents’ Professional Growth Through Workplace Relationships. Please go read this impressive work here. This picture shows the all female research team: dr Milou Silkens, PhD en dr Renee Stalmeijer, PhD as Iris co-supervisors, and myself as Iris proud supervisor.
What a great start of the week! I feel honoured to be presented as the newest board member of the Dutch Network of Women Professors (LNVH). Thank you LNVH for this important position. Please be assured of my enthousiasm for and commitment to further strengthening the position and professional fulfilment of women (of all backgrounds) in academia!
Gender equality is not ‘just’ about equal representation of women in all positions, and in particular in positions of power. Ultimately it is about justice. Women are still experiencing a gender gap to the invisible but undoubtedly masculine norm in academia: in the way we treat female academics, organise our institutions and value our researchers. Let’s get to work!
The feminist novelist Virginia Woolf once observed, “Science, it would seem, is not sexless; she is a man.” In the same spirit, one could argue that medicine is not gender-neutral — she is male. This is what we come to conclude in our paper published today in the New England Journal of Medicine. ‘We’ here is my co-author, Stanford physician and novellist Abraham Verghese, and myself. We hope our work will be supportive of the much-needed dialogue about today’s gendered medicine.
The world around us is constantly changing. Digitization, individualization, acceleration, feminization, robotization, and other societal developments have a significant impact on healthcare and the training of doctors and other healthcare professionals. The (In)Sanity in Healthcare Symposium – June 16th 2022 – revolves around the question which developments to embrace and which to be more critical of and/or cautiously monitor. Against this backdrop we focus on the topics of professionalism, vitality, and compassion. The Symposium is Dutch spoken, with the exception of the keynote lecture given by Canadian McGill University and dear personal friend Professor Yvonne Steinert, a world renowned expert in the field of medical education and training.
 All good things must come to an end. I am deeply grateful for the CASBS experience. What a absolutely transformative year it has been. Thank you my dear fellow class mates and thank you wonderful staff of Stanford University’s Centre for Advanced Study in the Behavioural Sciences. Thank you Margaret Levi for your leadership in this very challenging year, and allways. A big thanks also to Stanford Medicine’s Presence Program and in particular my host and dear friend Abraham Verghese.
All good things must come to an end. I am deeply grateful for the CASBS experience. What a absolutely transformative year it has been. Thank you my dear fellow class mates and thank you wonderful staff of Stanford University’s Centre for Advanced Study in the Behavioural Sciences. Thank you Margaret Levi for your leadership in this very challenging year, and allways. A big thanks also to Stanford Medicine’s Presence Program and in particular my host and dear friend Abraham Verghese.
I will continue my studies and hope to see you all again soon. Miss you already!
 Today, the LNVH presented the Monitor of Women Professors 2025 in the auditorium of TU Delft. Chair Prof. Yvonne Benschop outlined the main figures and symbolically presented the first copy to the university’s Vice-Rector, Prof. Hans Hellendoorn (see photo).
Today, the LNVH presented the Monitor of Women Professors 2025 in the auditorium of TU Delft. Chair Prof. Yvonne Benschop outlined the main figures and symbolically presented the first copy to the university’s Vice-Rector, Prof. Hans Hellendoorn (see photo). How do residents learn to become compassionate healthcare providers? Doctors – and patients! – consider compassion to be an important aspect of patient care, yet the subject of ‘compassion’ is not part of the medical curriculum. In practice, residents often learn a great deal by ‘observing’ their supervisors; modeling behavior thus becomes an important teaching strategy. In this study, we examined whether medical residents observe compassionate behavior in their supervisors and to what extent they view their supervisors as role models. Furthermore, we were interested in whether residnets observed differences between female and male supervisors. The good news is that, in general, residents positively evaluate the compassionate behaviors of their supervisors. Moreover, supervisors who received higher ratings from residents for ‘showing compassion toward patients and their families’ were also more often seen as role models by residents. Interestingly – and in line with socio-historical gender expectations – female supervisors scored significantly better in displaying compassionate behavior, but male supervisors received more appreciation for demonstrating compassion. For further reading, see
How do residents learn to become compassionate healthcare providers? Doctors – and patients! – consider compassion to be an important aspect of patient care, yet the subject of ‘compassion’ is not part of the medical curriculum. In practice, residents often learn a great deal by ‘observing’ their supervisors; modeling behavior thus becomes an important teaching strategy. In this study, we examined whether medical residents observe compassionate behavior in their supervisors and to what extent they view their supervisors as role models. Furthermore, we were interested in whether residnets observed differences between female and male supervisors. The good news is that, in general, residents positively evaluate the compassionate behaviors of their supervisors. Moreover, supervisors who received higher ratings from residents for ‘showing compassion toward patients and their families’ were also more often seen as role models by residents. Interestingly – and in line with socio-historical gender expectations – female supervisors scored significantly better in displaying compassionate behavior, but male supervisors received more appreciation for demonstrating compassion. For further reading, see  I wish you happy holidays and a new year filled with POSITIVITY. Reading the news, it’s clear we could all use a little more of it. And in my personal life too, I often hear too much negativity. A positive life isn’t just more fun and enjoyable—it’s also, as scientists show, better for our relationships, well-being, and happiness.
I wish you happy holidays and a new year filled with POSITIVITY. Reading the news, it’s clear we could all use a little more of it. And in my personal life too, I often hear too much negativity. A positive life isn’t just more fun and enjoyable—it’s also, as scientists show, better for our relationships, well-being, and happiness. Some studies reach the heart just a bit more deeply than others. This study is one of those, and it just so happens to be about the heart. The warm heart, the compassionate heart, the heart of healthcare professionals that beats for their patients.
Some studies reach the heart just a bit more deeply than others. This study is one of those, and it just so happens to be about the heart. The warm heart, the compassionate heart, the heart of healthcare professionals that beats for their patients. When I began developing the SETQ system over 15 years ago (The system that evaluates the teaching qualities of supervisors in residency training programs, and provides them with feedback), I could not have anticipated that one day there would be a Brazilian version. The fact that SETQ Smart is now being used in Brazilian residency programs is thanks to the vision, determination, enthusiasm, and dedication of Brazilian family physician and researcher Dr. Naarai Comboin Bezerra. Since our first email contact in 2019, the connection between Amsterdam and Florianopolis has only grown stronger. This publication in Brazil’s leading medical education journal is one of the outcomes of our collaboration. The publication (SETQ Brazil 2024) demonstrates the importance of ongoing validation of (social science) tools in the context in which they are used. Naarai is now temporarily with us in Amsterdam as a visiting scholar. She has become a valuable member of the team, and I enjoy all the cross-cultural lessons she teaches us daily. Read the article
When I began developing the SETQ system over 15 years ago (The system that evaluates the teaching qualities of supervisors in residency training programs, and provides them with feedback), I could not have anticipated that one day there would be a Brazilian version. The fact that SETQ Smart is now being used in Brazilian residency programs is thanks to the vision, determination, enthusiasm, and dedication of Brazilian family physician and researcher Dr. Naarai Comboin Bezerra. Since our first email contact in 2019, the connection between Amsterdam and Florianopolis has only grown stronger. This publication in Brazil’s leading medical education journal is one of the outcomes of our collaboration. The publication (SETQ Brazil 2024) demonstrates the importance of ongoing validation of (social science) tools in the context in which they are used. Naarai is now temporarily with us in Amsterdam as a visiting scholar. She has become a valuable member of the team, and I enjoy all the cross-cultural lessons she teaches us daily. Read the article